Pain sits at the crossroads of physiology, psychology, and context. It can be a broken wrist in a schoolyard, a neuropathic shed that remains long after shingles, the hurting spine that keeps a nurse off the lineup, or a post‑operative person grimacing behind a stoic face. A solid pain management accreditation program transforms that intricacy into useful proficiency. It develops the practices that clinicians carry to the bedside, to the ambulance bay, and to the area. It is not a badge, however a scaffolding for judgment, safety, and empathy.
This overview unpacks the proficiencies every reputable certificate program hurting management should show, exactly how those skills convert to daily practice, and exactly how to choose a training course that fits your extent and setup. It also attends to particular streams such as discomfort monitoring courses for nurses and discomfort administration programs for physio therapists, in addition to brief training courses in pain monitoring that target emergency situation care.
What a discomfort administration qualification ought to cover
The best programs anchor themselves to proof while equaling practice. Concept matters, yet only insofar as it changes what you do at the client's side. Whether you choose a pain monitoring certificate program developed for acute treatment, community health, or rehab, seek the following motifs woven via the curriculum.
Assessment as a professional skill. Exact pain analysis is more than requesting a number. It is selecting the appropriate device for the client in front of you, observing habits, and readjusting for cognitive impairment, developing phase, culture, and language. Grownups who lessen distress require a different method from an anxious teenager or a nonverbal older adult with ecstasy. A robust pain administration training block offers you a toolkit: numeric scales, spoken descriptors, visual analog scales, Wong‑Baker for pediatric medicines, PAINAD for mental deterioration, and function‑oriented questions like, "What can you do since you couldn't do yesterday?" Competent clinicians triangulate across these.
Pharmacology with guardrails. Drug is not a monolith. Non‑opioids, opioids, adjuvants, topical representatives, and local methods all have a place when utilized deliberately. Excellent pain administration training programs show dose titration, ceiling impacts, opioid similarities, cross‑tolerance, body organ problems adjustments, and interactions. They likewise instruct restraint: when to stop, when to trial nonpharmacologic therapies first, and just how to deprescribe without triggering withdrawal or rebound pain.
Nonpharmacologic therapies that really get made use of. Way too many programs pay lip solution to warmth, ice, placing, workout treatment, or cognitive techniques. The helpful programs demonstrate exactly how to make them stick in actual clinics: establishing person expectations, creating micro‑goals, scripting useful training, and documenting end results. For physio therapists, discomfort monitoring programs for physio therapists ought to relocate beyond tissue‑centric designs to modern pain scientific research, graded exposure, pacing, and interaction that pacifies threat.
Communication that constructs partnership. Words we choose can get worse or lighten discomfort. Avoiding catastrophic language, verifying the person's experience, and setting truthful goals modifications adherence and stress and anxiety. This is especially crucial in emergency discomfort management, where minutes matter and depend on establishes whether a person will accept a nerve block, inhaled analgesia, or a single‑dose opioid.
Safety, threat mitigation, and stewardship. No certificate training course hurting administration is total without functional danger evaluation for abuse, overdose avoidance, naloxone education, and risk-free storage space. This is not simply for opioid therapy. Gabapentinoids, NSAIDs, and tricyclics carry risks too, especially in polypharmacy. Programs must cover monitoring strategies, prescription medicine tracking databases where suitable, and recommendation thresholds.
Special populations. Youngsters, expectant individuals, older grownups, individuals with kidney or hepatic impairment, those with OSA, and patients with material usage disorders all need tailored analgesic strategies. Discomfort administration courses for registered nurses and interprofessional groups must install these scenarios in simulation and instance testimonial, not just in slides.
Documentation that safeguards and informs. Clear, contemporaneous notes decrease mistake and assistance connection. High‑quality discomfort monitoring training for nurses and allied clinicians should develop habits like videotaping pain intensity and useful influence, interventions offered, time to effect, damaging results, and follow‑up steps.
Across these styles, the programs that stand out set didactic web content with case‑based understanding, micro‑simulations, and reflective debriefs. They give you sample expressions for difficult discussions and design templates you can adapt to your setting.
Matching qualification to your function and environment
A solitary training course can not offer every person equally. A rural paramedic needs various devices from an outpatient physio or an oncology nurse. When examining a discomfort administration accreditation course, very first map your day‑to‑day demands.
Ambulance and first reaction. Paramedics and initially responders often take advantage of brief training courses suffering management focused on quick assessment and area treatments. In some areas, the PUAEme008 Provide Pain Management unit (typically written as PUAEME008 Give Pain Management in competency structures) specifies the standard for prehospital analgesia. It typically covers nitrous oxide/oxygen mixes, methoxyflurane where permitted, fundamental opioid administration under procedures, and nonpharmacologic approaches like splinting and positioning. The best implementations stress scene security, authorization, and review every few minutes. If your service is upgrading procedures, a targeted emergency situation pain monitoring training course can re‑align practice swiftly.
Acute care nursing. Pain administration training for nurses in hospitals must prioritize post‑operative paths, multimodal analgesia, PCA safety, nerve block aftercare, and recognition of red flags concealed by anesthetics. Graveyard shift facts belong in the curriculum: just how to titrate safely when staffing is lean, how to intensify when a block disappears at 3 a.m., and exactly how to record sedation ratings along with pain scores.
Primary treatment and community health. For generalists, a pain monitoring certificate oriented to chronic non‑cancer pain is commonly most useful. It ought to attend to graded task, quick behavioral treatments, rest health, neuropathic pain regimens, and exactly how to have actually structured opioid testimonials without rupturing connection. Recommendation mapping issues right here: knowing who in your area takes complex situations and what details they need.
Rehabilitation and physiotherapy. Discomfort management courses for physio therapists need to integrate modern pain neuroscience with hands‑on method. Graduates must be able to clarify sensitization without jargon, established direct exposure pecking orders for fear‑avoidance, and companion with prescribers to taper medicines while raising feature. Programs that consist of role‑play around language selection help medical professionals avoid nocebo impacts from laid-back remarks.
Palliative and oncology settings. Medical professionals Click for more require deepness in opioid rotation, case discomfort planning, adjuvants like ketamine or methadone under expert assistance, and the values of balancing awareness with comfort. Documentation and household communication are as essential as titration.
Your extent and guidelines determine what you can do. A trustworthy discomfort management qualification training course will certainly note plainly where regional regulations form method, for example who may provide methoxyflurane, start a PCA, or suggest adjuvants.
Building core proficiencies in assessment
Assessment is a living process. Discomfort modifications hour to hour with motion, mood, and therapy. Strong training programs show medical professionals to use both ranges and stories.
A fast instance from the ward: a client with an overall knee replacement reporting 7 out of 10 at rest. Standard reflexes might cue much more opioids. A more nuanced analysis notes that the patient can execute straight‑leg raises and rest beside the bed for only one min before quiting due to pain and anxiety. After coaching, ice, a little opioid top‑up, and an adjustment ready, the number at remainder continues to be 6, but the client currently tolerates five minutes of mild activity and approves physio. Function enhanced while the number barely moved. Without a function‑oriented framework, you may miss that progress.

In prehospital care, the evaluation window is pressed. Paramedics have to infer severity from device, vitals, motion, and quick discussion. The PUAEME008 Offer Pain Monitoring expertise, where taken on, trains -responders to examine contraindications quickly, make use of structured devices like AVPU and sedation scales, reassess every five minutes, and paper both the strength and the action to interventions. That rhythm prevents under‑treatment and over‑treatment.
For kids, the ability hinges on blending monitoring with developmentally appropriate ranges. A six‑year‑old post‑fracture might rate discomfort as "huge" or "small" on a faces scale. The clinician likewise sees limb guarding, play habits, and consolability. Pediatric doses are weight based and timing delicate. A good discomfort management course offers you mental mathematics shortcuts, pre‑calculated graphes, and exercise with carers that fear yet important allies.
Cognitive impairment complicates self‑report. In elder treatment, devices like PAINAD combined with family input and mindful trialing of analgesia can disclose distress masked as "frustration." Courses that consist of video clip vignettes have a tendency to prepare medical professionals much better for these subtleties.
Multimodal analgesia as default, not exception
Single agent strategies are simple to show and document yet rarely ideal. A multimodal strategy strikes various pain pathways with lower dosages, reducing damaging impacts. In surgical wards, that might be routine paracetamol, an NSAID if renal feature enables, a low‑dose opioid for innovation, regional anesthetic where offered, and very early mobilization under physiotherapy. In neuropathic pain, it could be a gabapentinoid or SNRIs, topical lidocaine, and paced task. In emergency pain monitoring, it might be splinting, nitrous or methoxyflurane for fast relief, and a tiny IV opioid dose in a titrated fashion.
The technique is to prevent polypharmacy without objective. Programs worth their cost educate you to set a stop date for every single prn, strategy testimonials, and expect duplication throughout discharge recaps and community prescriptions. They likewise emphasize bowel routines together with opioids and renal surveillance when NSAIDs are utilized beyond a couple of days.
Regional methods should have even more interest generally training. Even if you do not perform blocks, recognizing their indications, advantages, and red flags assists you supporter for clients and monitor them securely. For registered nurses, a discomfort administration training course that consists of catheter look after continuous nerve blocks, fall threat payments, and paperwork of motor and sensory changes is gold.
Communication that reduces pain
Words transform physiology. A basic "your discomfort is actual and we are going to treat it with each other" decreases anxiousness and muscle tension. Explaining what to expect from a medication-- "this will likely take 15 minutes to start aiding, and your discomfort should be half what it is currently"-- lowers the perception of delay and offers a timeline for alleviation. In persistent discomfort, reframing from "we will get rid of pain" to "we will increase what you can do, even if some pain remains" protects against disappointment and opens the door to rehabilitation.
I keep a short script for difficult discussions concerning opioids. It acknowledges the client's suffering, links safety to operate, and uses substantial options. Role‑play in a pain management certification program helps clinicians locate language that fits their style while avoiding adversarial characteristics. In our service, a quick exercise transformed how colleagues responded to the inquiry, "Are you calling me a drug hunter?" The brand-new answer-- "I am calling you a person in pain, and my work is to make a secure strategy that assists you now and protects you later"-- pacified a number of stressful experiences on the spot.
For physio therapists, discomfort education and learning calls for treatment. Avoid stating "your back is unsteady" or "your knee is damaged" unless imaging and function require it. Phrases like "sensitive, not damaged" paired with graded exposure can move habits. Excellent pain administration courses for physio therapists consist of patient‑tested allegories and approaches to customize descriptions to personality and culture.
Risk administration without stigma
Risk screening is part of thoughtful care. Tools and checklists assist, but the tone matters. Asking, "Has any person in your home ever required aid with medication safety?" defeats a cold "Any kind of history important misuse?" It opens a discussion regarding storage space, kids in the home, and safe disposal. In setups where naloxone is readily available, normalizing it as a seatbelt rather than a label lowers resistance.
Courses ought to show functional systems that safeguard every person: double checks for high‑risk application adjustments, independent sedation scoring before repeat opioid doses, infusion pump safeguards, and acceleration triggers. For ambulatory practice, arrangements that concentrate on goals and safety instead of penalty often tend to work better.
Be alert to non‑opioid dangers. NSAIDs can speed up kidney injury in dehydrated clients, intensify cardiac arrest, and cause GI blood loss. Gabapentinoids increase sedation and falls when integrated with opioids, especially in older grownups. Tricyclics help neuropathic pain yet intensify orthostasis and anticholinergic concern. A well‑designed pain monitoring certification program drills these warns right into reflex.
Documentation as a clinical tool
Documentation is not a duty when you treat it as component of the treatment. A solid note communicates trajectory and issues to the next clinician. In method, that looks like this: "Pain 8/10 at rest, securing right reduced limb. Methoxyflurane self‑administered for 4 minutes, splinted shin, advised in slow breathing. Pain 4/10 on activity after 7 mins. No nausea. Vitals secure. Plan: titrate fentanyl 25 mcg IV if pain remains over 5 throughout extrication. Reassess every 5 minutes." That degree of clearness stops over‑dosing, flags the next action, and works as a mentor artifact later.
In wards and centers, pair intensity with feature: "Can walk 20 meters with frame prior to quiting as a result of pain at the cut. No sedation. Bowel opened today. Will add normal paracetamol 1 g q6h, proceed advil 200 mg q8h with food for 48 h, oxycodone 5 mg prn for innovation as much as 20 mg per day. Objective for tomorrow: 40 meters."
Pain administration training for registered nurses should consist of graph audits and feedback. It is humbling the very first time, then promptly ends up being enjoyable as you see patterns and close loops.

Choosing the best training course: what to look for
Clinicians run into a congested market of pain monitoring training courses. A fast list can conserve time and money.
- Clear positioning with your extent, including authorized medications or methods you can make use of, and practical instance circumstances from your setting. Faculty who still practice scientifically and can answer "what do you do when" concerns with specifics, not theory. Assessment that checks judgment under constraints, not simply recall. OSCEs, simulations, or instance write‑ups are much better than multiple choice alone. Practical sources you can take back to function: application graphes, client handouts, scripts, and paperwork templates. A plan for maintenance of capability, whether routine refresher courses, updates on standard adjustments, or chances for instance discussion.
Programs that prepare paramedics for PUAEME008 Provide Pain Administration or comparable proficiencies must consist of device labs, substitute loud settings, and repeating under time stress. Hospital‑oriented courses ought to include PCA pump troubleshooting, post‑block surveillance, and after‑hours rise pathways. For discomfort monitoring programs for physiotherapists, ask whether the mentor includes graded exposure planning, flare‑up administration, and interaction mentoring, not just composition refreshers.
The anatomy of an efficient brief course
Short training courses in pain monitoring can provide outsized gains if they are firmly focused. A two‑to‑eight‑hour emergency situation discomfort monitoring component can change practice in a solitary shift.
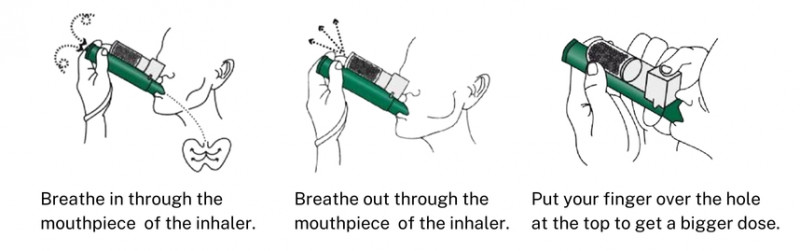
Consider a half‑day program for blended ED personnel. In the first hour, upgrade on rapid analgesia pathways: triage‑initiated paracetamol and advil for crack patients without contraindications, IN fentanyl methods, and the role of ketamine for severe pain with hypotension dangers. The 2nd hour, run simulation: a screaming toddler with a forearm crack, a stoic older adult with a hip crack and borderline oxygen saturation, a patient in sickle cell dilemma ranked as tough by the last team. Include methoxyflurane mouth piece setting up and troubleshooting. The third hour, debrief documents and bias. Who got analgesia fastest, and why? Where did language or assumptions postpone treatment? Do with a fast expertise check and a one‑page method card. That framework sticks.
On the other end, a pain monitoring certificate designed for area care could run over a number of weeks with online components and live workshops. The most effective ones assign 2 patient cases that individuals track over a month. You see the messiness of good days and flare‑ups, medicine modifications, and rehab pacing. The knowing ends up being local, not abstract.
Implementing brand-new abilities on the floor
One course does not eliminate old routines. Turning accreditation right into technique takes purpose and team buy‑in. I have actually seen solutions pair training with small system fine-tunes that make change likely. Equipping nitrous or methoxyflurane in grab bags so teams do not need to unlock additional closets boosts usage when proper. Revising admission order sets to include multimodal analgesia with quit days and bowel routines moves recommending patterns. Including a discomfort review area to electronic records requires a moment of representation and documentation.
For physiotherapists, straightforward devices assist. A one‑page flare‑up plan that people can complete-- what to do, how to scale back, when to call-- decreases anxiety and unplanned check outs. A language overview taped to the desk converts professional lingo right into individual expressions that lower threat. In time, you see fewer no‑shows and far better adherence.
Nurses often become the very early warning system. A common expression like "Sedation score 2 prior to prn demand" in handover sets off a conversation with the prescriber. A shared sight of what "breakthrough discomfort strategy" implies avoids the back‑and‑forth at 2 a.m. where everybody is presuming. Pain administration training for registered nurses ought to show not only the web content, however also how to lead these micro‑improvements on the unit.
Evaluation and maintenance
Certification needs to mark the beginning of a learning cycle, not its end. Discomfort scientific research evolves, medications come and go, and individual expectations change. Develop a basic review rhythm. Every quarter, pick one theme-- for example, neuropathic pain regimens-- and examine five cases. Did the plan match guidelines? Were adverse effects tracked? Did function improve? Share searchings for in a short huddle. The point is not conformity cinema. It is to catch drift and reinforce great habits.
Refresher pain monitoring training programs do not need to be long. A 60‑minute upgrade on new support, a debrief on a tough case, and a fast skills check for any tool keeps capability fresh. Providers lined up to PUAEME008 offer discomfort administration often require regular recertification. If you deal with the process as a possibility to improve procedures and debrief real incidents rather than a box‑tick, your crews will engage.
Ethics and equity
Pain is not dispersed rather. Predisposition permeates in. Research studies regularly reveal that people from marginalized groups get less analgesia for comparable problems. Qualification programs need to challenge this clearly. Instruct groups to utilize structured devices to reduce subjective drift, pain management certification workshops and to take a look at where presumptions alter decisions. In practice, this may mean applying triage‑initiated analgesia methods that do not wait on a physician's assessment, or producing standing orders that encourage registered nurses to begin non‑opioid treatment and nonpharmacologic actions quickly.
Language accessibility is essential. Pain analysis loses precision with bad translation. Services that purchase interpreter gain access to, simple patient handouts alike languages, and staff training in plain speech see much better end results. In physiotherapy, culturally adapted discomfort education products enhance interaction and trust.
Ethics additionally indicates limits. Learn to claim no to harmful requests in a manner that maintains the relationship undamaged. A pain administration certification training course that includes role‑play with standardized clients and responses will aid you locate words that value autonomy while securing people and the public.
A note on law and credentials
Before joining, verify that the discomfort monitoring qualification lines up with your territory's guidelines. Some certifications carry CPD or CME credits, others satisfy details expertise devices like PUAEME008 Provide Pain Management for emergency situation solutions. For prescribers, examine whether conclusion fulfills neighborhood board expectations for opioid suggesting training. For nurses and physio therapists, verify that the course is identified for expert development hours and pertinent to your scope.
Marketing can be noisy. Look past buzzwords and find the alignment with your daily job. Request for a curriculum. If a carrier can not tell you exactly how their discomfort management certificate prepares you for the situations you encounter most, maintain looking.
What changes on Monday morning
The ideal feedback I listen to after a solid discomfort management course is simple: "I dealt with pain quicker," or "My individual walked further," or "That discussion went much better." Accreditation materializes when clients feel relief quicker, when unfavorable occasions drop, and when your notes tell a story that any kind of coworker can follow.
A paramedic staff chooses splinting and methoxyflurane during a difficult extrication, reflects on, then adds a tiny opioid dose. The individual gets here calmer, with steady vitals and no nausea or vomiting. A surgical registered nurse pairs regular non‑opioids with an early bowel program, trains mobilization, and restricts prn opioids to function‑limiting discomfort. A physiotherapist clarifies pain sensitization in simple language and builds a rated plan that the person relies on, with a flare‑up strategy taped to the refrigerator. These are the results that matter.
Pain monitoring accreditation is not regarding excellence. It has to do with constructing the habits that make good decisions likely under stress. Pick a program that hones your judgment, practice the skills till they are tranquil reflexes, and maintain refining. Patients feel the difference.